⦿ AI Agents For Prior Authorization
Automate Pharmacy Operations Using AI-Powered Prior Authorization
Prior Authorization Challenge
Complexity
Varying payer rules and documentation requirements.
Delays
Prolonged wait times for medication approval.
Resource Drain
Significant staff time and resources for manual processes.
Patient Impact
Treatment delays, increased out-of-pocket costs, and potential non-adherence.
Solutions for Intelligent Prior Authorization
AI-Powered Data Extraction
Automatically pulls patient and prescription data from various sources.
Smart Form Filling
Populates prior authorization forms accurately and efficiently.
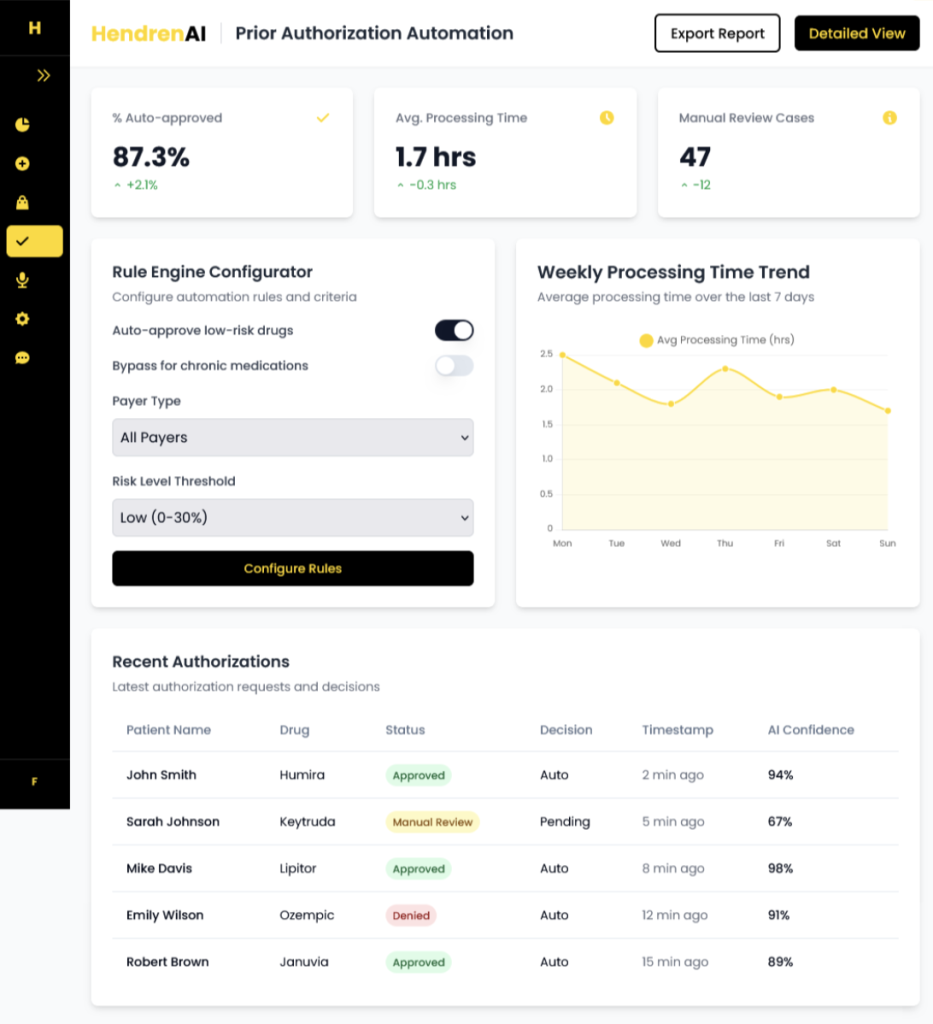
Rule-Based Engine
Applies payer-specific rules to ensure compliance and reduce denials.
Automated Submission
Streamlines the submissions process to payers.
Real-time Tracking
Provides visibility into authorization status, reducing follow-up calls.
Automate Outbound PA Calls
Proactive AI-driven calls to payers or patients for PA status updates or missing information.
AI-Powered Prior Authorization
AI-Powered Prior Authorization platform revolutionizes the approval process by enabling 85% automated decision-making with just 15% human oversight. This intelligent system significantly reduces administrative costs, streamlines workflows, and eliminates manual errors, ensuring faster and more accurate approvals.
- Reduce Administrative Costs
- Streamline Processes
- Eliminate Manual Errors
- Prevent Delays
- Maintain Oversight
Start Your AI Journey
Contact Us
- Send a Message
- Your information is secure and encrypted



